Have a story about challenges with PPE while working in healthcare during COVID19? Congress wants to hear from you!
Senate Finance Committee Ranking Member Ron Wyden, D-Ore., is asking for health care workers to submit their experiences trying to obtain personal protective equipment (PPE) during the COVID-19 pandemic.
“I want to hear the stories of the people being affected by these shortages—nurses, EMTs, doctors and health care providers struggling to get PPE. Lifting up these stories in the coming weeks will be crucial to Congress’ understanding of the work ahead.”
Stories can be emailed to PPEshortages@finance.senate.gov. The deadline for submissions is August 31st. All personal information will be redacted unless requested otherwise
This is your chance to have your stories, your stress, and your frustrations heard. I shared my story. I would love to have our collective stories shared to see if we can make a difference in the availability of PPE for all frontliners in the United States.
- Sarah @ New Thing Nurse
Here is the testimony I sent to Senator Ron Wyden via my emergency nurse colleague, Penelope Blake:
“My name is Sarah K. Wells, MSN, RN, CEN, CNL. I am a Registered Nurse who has worked in emergency and radiology medicine since 2010. I live in Oakland, California and work at two hospitals in the Bay Area.
I am writing to you today to share my experiences with the Personal Protective Equipment (PPE) shortages that are facing the frontline healthcare workforce in the United States. For nearly 10 years, I have worked in the hospital setting. As a nurse, I come to work each shift to care for those in need. In the emergency department, I see patients from newborns to the elderly and am responsible for being able to care for minor to the most complex medical conditions in collaboration with interdisciplinary care teams. I am trained to respond to disasters in often hazardous conditions and have learned to utilize a wide variety of PPE to prevent exposure to infectious diseases and hazardous materials. From being trained to care for patients with Ebola to those suffering from chemical burns, I know that I must protect myself so that I can care for others.
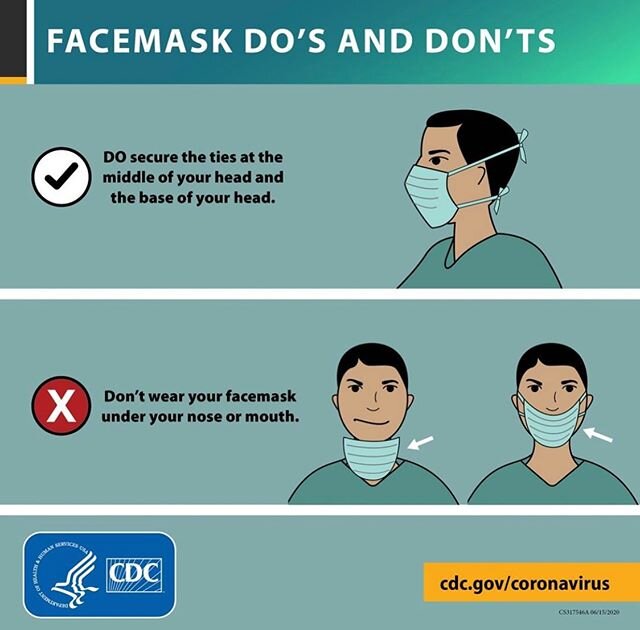
The majority of the PPE that I am trained to use is single-use, single-patient items. This means that I would wear PPE for use with one patient encounter and then dispose of it. Imagine a patient with tuberculosis, an infectious disease spread through airborne transmission. Historically, I would have that patient in a private, isolation room in the emergency department. To enter the room safely and care for the patient, I would put on a N95 respirator mask, a specialized mask that filters out approximately 95% of airborne particles, along with other appropriate, single-use PPE per my facility's policy, enter the room, complete my patient care, exit the room, and throw that N95 respirator mask and other PPE away in the trash. I would then perform the appropriate hand hygiene and move on with my work day. Whenever I needed to re-enter that patient's room, I would then put on a fresh N95 respirator mask and PPE, complete the necessary care, and dispose of PPE upon every exit from the patient's room. In this way, I never put on "dirty" masks or other equipment, meaning masks that have been exposed to germs from previous encounters in the tuberculosis patient's room. I never risk exposing myself to that patient's germs by putting on the "dirty" PPE, and I would never wear "dirty" PPE into another patient's room. I have gone through dozens of masks per shift in the past without thinking twice because it was the standard of safety and best care for my patient and the policy of my employer.
All of that changed this year when COVID-19 came to the United States. In March, early rumors of N95 respirator mask shortages started to circulate. Then there was discussion that we may need to start extending the use of our single-use N95 masks. This seemed impossible. How could we re-use a single-use item? It went against our infection prevention policies and put us at risk for exposure to infectious germs. I assumed this was just talk until my emergency nurse colleagues from across the United States started to tell me that it was true and happening. And soon, it was not just re-using the N95 masks for a few hours, but the whole shift, and then multiple days. By the end of March, I had colleagues telling me that they were using the same N95 masks for weeks at a time. And then, I was told by many friends and acquaintances that nurses and other medical staff were caring for COVID-19 patients with no N95 masks at all because there were none to be had. This would have been an unacceptable situation in January and now, it was becoming the norm.
At my facility in California, we did not face this reality until sometime in April. We have thankfully never completely run out of N95s. However we have been encouraged to extend the use of our single-use N95s for multiple shifts, being given cardboard containers that you would normally use in our cafeteria to get a hamburger to-go, to store our masks in between uses. Our emergency department, like most in the United States, also has a limited amount of Power Air Purifying Respirators (PAPRs) units, battery powered machines that are attached to plastic hoods, that can be used for working safely with COVID-19 patients. However these units are expensive and most emergency departments only have a hand full. These are sufficient for caring for small numbers of patients, but not for managing large quantities of COVID-19 patients all at once. And then there are emergent situations, for example where a person's heart stops and a team of people are needed in the room to perform life-saving measures, you may need 3 to 5 PAPRs at the same time for just one patient. That can easily be the department's entire supply of PAPRs. If a department is out of N95 masks and all the PAPRs are in use in one room, there is no way to safely care for the dozens to hundreds of other COVID-19 patients that you may have at the moment in your emergency department.
Furthermore, there is the rest of the hospital to consider. While the emergency department is specially trained to handle disasters headon with advanced PPE and a supply of PAPRs at the ready, most inpatient units have even less training and PPE supplies available. When COVID-19 initially hit, the majority of hospitals quickly depleted their PPE reserves and were scrambling to train all their staff to safely take care of our high-risk patients. And then the supply chain for PPE was broken, and facilities could not refill their supplies of PPE or procure more PAPRs. The inpatient units were caring for patients with not just re-used PPE, but insufficient PPE which put themselves and their patients at risk. Caring for a COVID-19 patient with a surgical mask is not safe because the surgical mask does not protect the person from COVID-19 exposure. Surgical masks only prevent my germs from spreading to others. And while many facilities are requiring all staff and patients to wear surgical masks, which in theory will greatly limit the spreading of germs, most of our hospital patients cannot keep a mask on due to their oxygen support needs, feeding tubes, anxiety, or confusion. Nurses and medical staff must have a N95 respirator at minimum to ensure they are not exposed to COVID-19 germs. This lack of PPE has had deadly consequences. Since this pandemic has started, there have been nearly 115,000 COVID-19 cases and nearly 600 deaths due to COVID-19 among healthcare workers in the United States.
In addition to being a practicing nurse in the hospital setting, I also am the Founder of New Thing Nurse, a company committed to supporting the nursing community through a variety of services and platforms. Through New Thing Nurse and my nursing professional organizations, I have contacts with nurses across the United States. When I started getting reports of the limited PPE in the United States, I started making calls and inquiries to see if I could find PPE sources for those in need. I quickly found that the normal sources for N95 respirator masks available to the public, such as hardware and paint stores, were completely out of inventory. I made contacts with hospital buyers, the staff in charge of stocking PPE for healthcare facilities, to see if there was a way that I could purchase N95 masks in bulk. I was quickly told that no sources were to be found.
I started reaching out to the community. I started receiving donations of PPE from individual citizens. People who had a few masks here and there for emergencies or painting projects. I started fundraising and putting small PPE orders together where I could find small sources online on the secondary market, from sources like Ebay and Craigslist, paying outrageous prices but getting small quantities of masks and other PPE items that were also becoming short supply.
To date, I have sent out and coordinated nearly 5,000 PPE items donations to frontline healthcare workers to 14 states with an estimated cost of $9,000+. I am just one small example of such an effort to keep friends, colleagues, and other medical workers in the appropriate PPE that they need to care for COVID-19 patients safely. Huge organizations like GetUsPPE.org and A Million Masks have emerged to raise hundreds of thousands of dollars and distribute millions of masks. These are projects created by private citizens to close a basic supply gap that employers and the government have failed to remedy. This failure has caused the illness and death of care providers across the United States, dedicated citizens who have devoted their lives to caring for others. While they were caring for us, we failed to care for them.
Here is one email that I received from a mobile x-ray technician in Texas who requested PPE from New Thing Nurse:
“Hello Sarah! I heard about you in the ... group on Facebook. It’s funny the timing as today after my shift I sat in my car and broke down crying.
I’m a mobile X-ray tech for ... in Texas. We service facilities, homes, long term care and jails all over Texas. Every single facility we service has Covid patients. Nursing homes and jails are especially rampant with it.
In the past three weeks there has not been one day I have done several x-rays on a positive patient. The majority of the facilities expect us as an outside contract to provide our own PPE. We are a very small company so finding them is scarce, I have been reusing the same gear several times over. My neighbor got me an N95 from her husbands laboratory. That’s how serious it is. Working at a small company we worry about publicly reaching out for PPE for fear of getting reprimanded. I don’t have anything negative to say about my employers, I honestly believe they are trying to get us PPE. But each day I literally go to work trembling worrying that it’s not going to be enough and I’m going to expose my family by not being adequately protected. I’m typing this in tears.
Today was an especially hard day as staff at one of the jails I was servicing were fighting over who was to receive a single mask. This is the same jail apart of a very large corporation that told me I needed to bring my own PPE but calls me everyday to image their Covid patients. Tensions were high and I reminded them we have to protect ourselves and our patients. There is a nurse who sneaks me PPE when she can, it is a very humbling experience to have to beg for that every shift. This is one of the most stressful times of my life. I will send my company info in the next email I’m typing on my phone.’’
The PPE shortage in the United States is a completely inexcusable failure. There is no reason that in a country as rich and powerful as ours that our medical workers should ever be without the appropriate equipment needed to provide the best and safest care to our patients. In the year 2020, healthcare workers have begged for PPE by going door-to-door in their communities, for PPE that should be provided as a standard workplace safety item by their employers. I implore you to take the necessary steps to finding a solution and keeping our frontline healthcare workers safe by providing appropriate PPE for all.’’